Contents:
- Medical Video: Breast Cancer in Pregnancy | Gina's Story
- Operation
- Anesthesia
- Postoperative treatment
- Chemotherapy
- Radiation therapy
- Hormone therapy
- Target therapy
- Breastfeeding while undergoing cancer treatment
- Plan treatment together
- The survival rate of pregnant women with breast cancer
Medical Video: Breast Cancer in Pregnancy | Gina's Story
Pregnancy together with breast cancer can occur even though this is quite rare. Breast cancer during pregnancy is caused by the presence of cancer hormones that trigger cancer, such as estrogen and progressesterone. Many pregnant women who also suffer from breast cancer prefer to delay the treatment of their disease. The reason, they were hit by fear of a treatment process that could threaten the health of the fetus if done while still pregnant. In fact, this myth is not true. Treating breast cancer, which is done as early as possible without waiting for the time of birth, will increase the chances of mother's life.
The type of treatment that will be given to pregnant women depends on several things, such as:
- Tumor size
- Tumor location
- Cancer spread
- Gestational age
- The choice of therapy desired by the mother
Treatment of breast cancer, both for pregnant and non-pregnant women, has the same goal, namely controlling cancer and preventing its spread. Only, the purpose of treatment will be more complex because the safety of the fetus in the womb must also be considered.
Breast cancer surgery is classified as safer than other treatments such as chemotherapy, hormone therapy, and radiation, because it can harm the fetus during pregnancy. For women who have breast cancer at the beginning of pregnancy and must immediately undergo chemotherapy, the doctor may recommend to end the pregnancy. For some types of breast cancer, such as inflammatory breast cancer, medical treatment must be done immediately so as not to endanger the patient.
One study found that ending pregnancy for undergoing cancer treatment did not improve a woman's prognosis. Although this study is not perfect, ending pregnancy is no longer recommended for breast cancer sufferers. However, this choice can be discussed after looking at all available treatment options, especially for aggressive cancers that may require immediate treatment. Pregnant women and families must know the benefits and risks of all treatment options before making a decision.
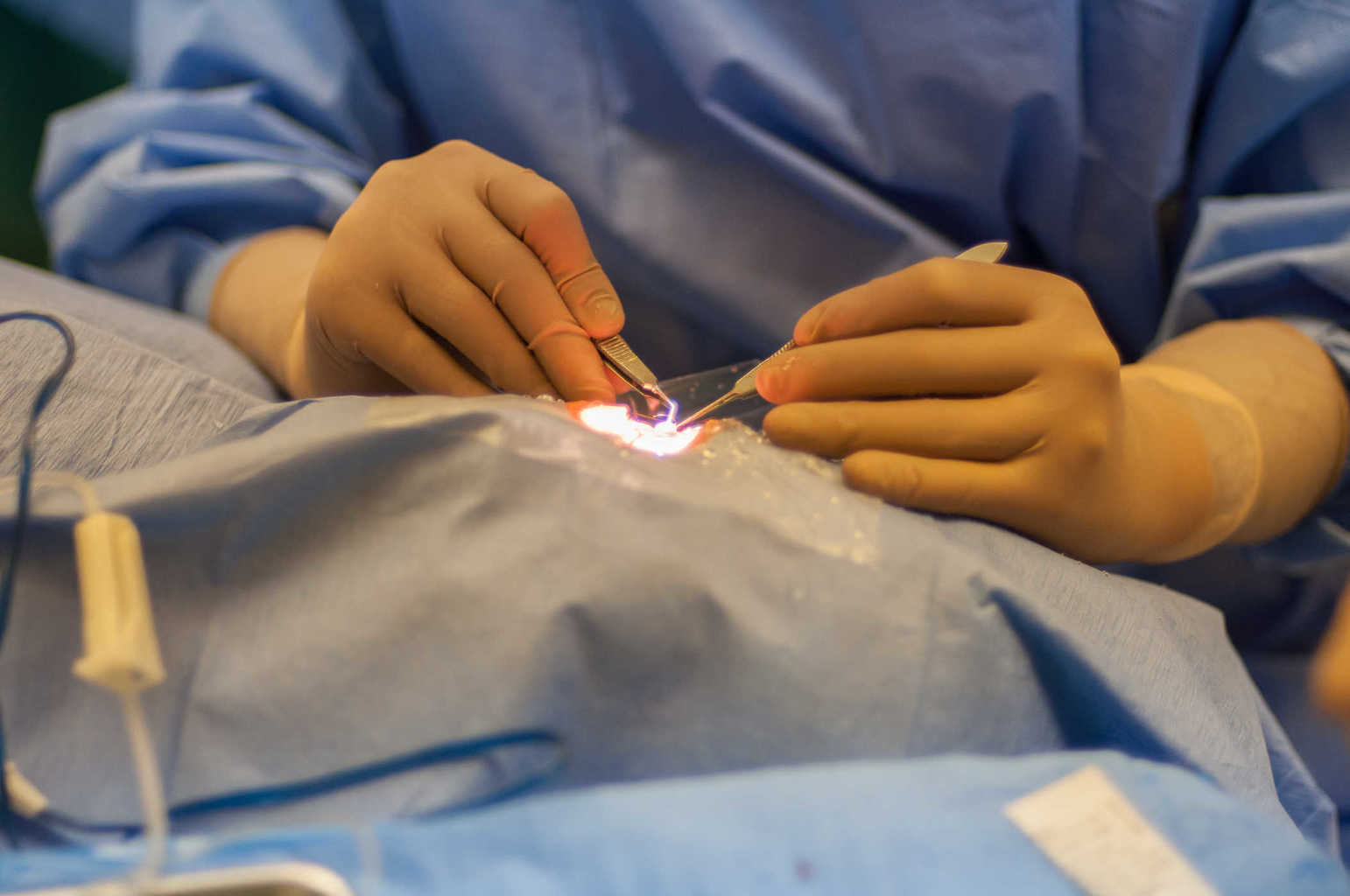
Operation
Surgery to remove cancer in the breast and around the lymph nodes is generally safe for pregnant women. Surgery is a major part of treatment for every woman with early breast cancer, including pregnant women. Surgery can be done by removing all parts of the breast (mastectomy) or only partially containing cancer (breast-conserving surgery - BCS). Compared to BCS, mastectomy is more often recommended for pregnant women because it does not require postoperative radiation therapy. Because the radiation can affect the growth and development of the fetus in the womb, so it cannot be given before labor. Delaying radiation for too long also increases the risk of cancer coming back. If cancer is found in the third trimester, radiation is usually given after chemotherapy (chemo), so patients who will undergo postoperative chemotherapy may not be able to delay radiation treatment. But if cancer is found early in pregnancy, radiation treatment can still be delayed. Cancer in early pregnancy is often treated with a mastectomy.
In addition to removing the tumor in the breast, the doctor will also remove one or more lymph nodes in the armpit to prevent the spread of cancer. One way to do this appointment is through axillary lymph node surgery (axillary lymph node dissection) This method removes many lymph nodes under the arm. Other procedures such as sentinel lymph node biopsy (SNLB) can be a choice of surgery, depending on the gestational age and stage of the cancer. This procedure uses a tracker and dye to determine the swelling that might contain cancer cells. SNLB allows the doctor to remove a little tumor. However, there are concerns about the negative effects of radioactive tracers and blue dyes used for SNLB in the fetus. Therefore, some experts suggest that SLNB is only used after the baby is born.
Anesthesia
Breast cancer surgery generally carries little risk to the fetus. But in some cases, anesthesia (anesthetic used during surgery) may even be risky for the fetus.
Various doctors, such as obstetricians, surgeons, and anesthesiologists, will discuss the right time for pregnant women to carry out surgery. In addition, doctors will determine the safest drugs and techniques for mothers and babies. If the operation is agreed to be carried out during pregnancy, the obstetrician will be alert to anticipate problems in the baby during surgery.
Postoperative treatment
Depending on the variety of cancer stages, patients can get further treatment, such as chemotherapy, radiation, and / or hormone therapy after surgery to help reduce the risk of cancer coming back. This treatment is called assisted treatment (adjuvant treatment) In some cases, this treatment can be delayed until the baby is born.
Chemotherapy
Chemotherapy, also called chemo, is an assisted treatment for several early stages of breast cancer. Chemo can also be used separately for further cancer stages.
Chemotherapy is not given during the early trimester of pregnancy because at this time most of the baby's internal organs are developing. The risk of miscarriage is also the most vulnerable in this period.
Recent research shows that certain chemotherapy drugs used during the second and third trimesters (4th to 9th months of pregnancy) do not increase the risk of birth defects, death, or health problems after birth, although chemo may increase the risk of preterm birth. However, researchers are still not sure whether these babies will have long-term effects or not.
When pregnant women with early breast cancer need to undergo chemo after surgery, usually chemo will be delayed until at least the womb age is in the second trimester. If cancer is found in the third trimester, chemotherapy may be delayed until the baby is born. In some cases, labor will be induced so that the baby can be born a few weeks earlier. Induction labor is also carried out in pregnant women with advanced cancer.
Chemo should not be given after 35 weeks of pregnancy or 3 weeks after delivery because it can reduce the amount of maternal blood. This condition can cause bleeding and an increased risk of infection during birth. Delaying chemo during the last few weeks before labor can restore the normal amount of maternal blood before giving birth.
Radiation therapy
Radiation therapy to the breast is often done after breast conservation surgery (lumpectomy or partial mastectomy) to help reduce the risk of cancer coming back. High-dose radiation used in this therapy can harm the fetus during pregnancy. This radiation can cause miscarriages, birth defects, slow fetal growth, or the risk of cancer in children. Therefore, doctors do not use radiation treatment for pregnant women.
Pregnant women who choose a lumpectomy or partial mastectomy may be able to undergo surgery during pregnancy and then wait until the baby is born before undergoing radiation therapy. However, waiting too long before undergoing radiation can increase the chance of the cancer coming back.
Hormone therapy
Hormone therapy is often used as a post-operative treatment or as a treatment for advanced breast cancer in people with type breast cancer receptor positive breast cancer. For early breast cancer, the drugs used include tamoxifen, anastrozole, letrozole, and exemestane. Other hormone therapy drugs can be used for advanced breast cancer.
Hormone therapy should not be undertaken by pregnant women because it can affect fetal development. This therapy can only be undertaken if the baby is born.
Target therapy
Types of drugs, such as trastuzumab (Herceptin®), pertuzumab (Perjeta®), ado-trastuzumab emtansine (Kadcyla ™) and lapatinib (Tykerb®), are important parts of the treatment for HER2 positive breast cancer in non-pregnant women. Trastuzumab is used as part of postoperative additional treatment. Trastuzumab can be used with pertuzumab before surgery, and all types of drugs can be used to treat advanced cancer. But based on research, these drugs are classified as unsafe for the fetus when consumed during pregnancy.
Everolimus (Afinitor®) and bevacizumab (Avastin®) can also be used to treat advanced breast cancer. Again, none of these drugs is safe to use during pregnancy.
Breastfeeding while undergoing cancer treatment
Women who have just given birth and will undergo breast cancer treatment are advised to stop breastfeeding.
Stopping breastfeeding will help reduce blood flow to the breast so that the size of the breast becomes smaller. Apart from helping the operation process, this can also reduce the risk of infection in the breast and prevent breast milk from accumulating in the operating area.
Drugs in target therapy, chemo, and hormones, can enter the baby's body through breast milk. Therefore, breastfeeding is not recommended for mothers undergoing target therapy, chemo, and hormone therapy.
Consult a doctor if you have questions about breastfeeding and therapy.
Plan treatment together
Determining the most effective treatment for mother and baby may be the most difficult part of a series of treatments. Make sure you consult with a specialist in making a decision. Obstetricians will work with surgeons, oncologists, radiation oncologists, and other medical personnel involved. For some mothers, the counselor or psychologist is also part of the health team to help provide the emotional support needed.
The survival rate of pregnant women with breast cancer
Diagnosis and treatment of breast cancer in pregnant women is more complicated. A study in 2013 looked at more than 300 pregnant women diagnosed with breast cancer. After 5 years of observation, this study compared the number of pregnant women with non-pregnant women who recovered from breast cancer (at the same stage). From the results of these comparisons, it is known that the number of pregnant women who recover tends to be lower.
For some doctors, ending a pregnancy is an attempt to slow the progression of breast cancer to an advanced stage, so this choice is sometimes recommended. However, it is actually difficult to prove the effectiveness of this method. Ending pregnancy may indeed make treatment simpler, but the results of previous studies have not shown an increase in the survival of pregnant women by ending pregnancy. Various factors may influence the results of the study so the results are invalid, for example pregnant women who are tested in research do indeed have a variety of serious complications so they must abort. Until now, no recent research has been found in the medical literature.
In addition, the study also did not show that delaying treatment (which is sometimes needed during pregnancy) will affect the results of cancer treatment. But again, the certainty of this assumption is difficult to examine.