Contents:
Medical Video: Hybrid Closed-Loop Insulin Delivery System: Top 10 Medical Innovations 2018
Artificial pancreas has long been the dream of researchers and people with diabetes. Although not perfect, the latest technological advancements bring the dream closer to reality.
For people with diabetes, especially those with type 1 diabetes, disease management is persistent. That's because the pancreas can't produce insulin, a hormone needed for life. Overcoming diabetes means getting involved with your own care every hour, every day, every year.
If you have diabetes, you must be careful in monitoring blood sugar levels, calculating how much insulin is used, and when to use it. Maybe you will need injections 2-4 times a day. Injections often hurt. Over time, it can also cause fat accumulation under the skin called lipohypertrophy. This condition makes it harder for your body to use insulin.
Many people with type 1 diabetes choose to use an insulin pump instead of injecting it themselves several times a day. The pump releases insulin throughout the day. With a pump, insulin is flowed through a catheter placed under the skin of the stomach. They can also press the button to release insulin after eating. However, people who use the pump must be careful with it and the channel must be removed when bathing or soaking.
Whether by pump or injection, the burden of disease management can be lighter. An artificial pancreatic system can help keep diabetes under control and reduce the possibility of complications. It can also relieve stress associated with insulin treatment and improve your quality of life.
How does the pancreas work?
The pancreas produces hormones, including insulin, which is a very important hormone. After you eat, the pancreas releases insulin into your bloodstream. Insulin helps convert your body's sugar (glucose) to energy. Insulin also makes your heart, muscles, and fat cells take excess glucose and store it until you need it.
Without insulin, glucose can accumulate in your blood (hyperglycemia). If not treated, high blood sugar can cause diabetic coma (diabetic ketoacidosis) and life threatening. The long-term risk of hyperglycemia includes heart disease, nerve damage, and kidney damage. When blood sugar is too low (hypoglycemia), you may have vision problems, feel trembling, and have unclear thoughts. This can make you pass out, convulsion, or coma.
This is the task of the pancreas to release insulin at the right time and only in the right dosage to prevent complications.
How will the artificial pancreas work?
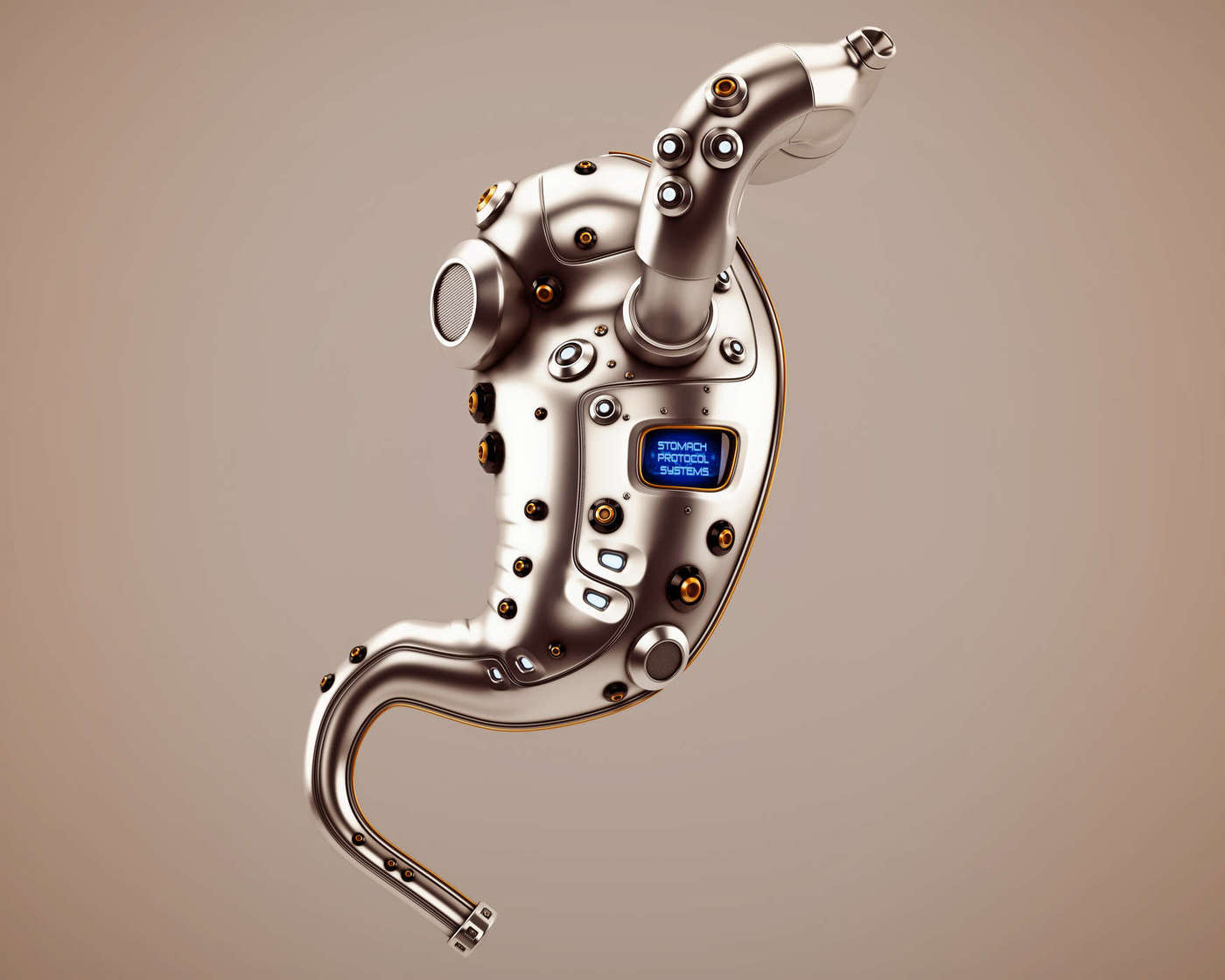
An artificial pancreas will not be like a natural pancreas. This tool does not become an internal organ. Instead, this device can be an external system that combines the work of a continuous glucose monitoring system with an insulin pump.
Two components of the artificial pancreas have been used. First, a continuous glucose monitoring system (CGM) checks glucose levels through sensors under the skin. CGM then sends the results to the wireless monitor. People who use CGM should check the monitor to find out if their glucose levels are too high or too low. They can also program the monitor to sound an alarm or read the tendency. Secondly, an insulin pump installed in the body can remove insulin throughout the day.
The third component is the most important for artificial pancreas. This is a technology that will allow CGM and insulin pumps to communicate with each other. This may sound simple, but designing this communication system is very complicated.
In an artificial pancreatic system, a glucose monitor will send information to an external controller equipped with an algorithm. Using an algorithm, the device calculates the dose needed and instructs the pump to give the right dose of insulin. Transfer of information between these devices will do the work of regulating insulin like a healthy pancreas. The margin for errors will decrease, and patients will be freed from the burden of making decisions.
Clinical trials with artificial pancreas are being carried out throughout the world. However, an effective system is not yet available. Even today the United States Food and Drug Administration has not approved this device for use in the United States.
What might happen in the future?
When it produces results, an artificial pancreas will not be a cure for diabetes. This tool will not eliminate the need to monitor or reduce the importance of diet and exercise to keep the disease well controlled.
However, this system can significantly reduce the risk of hyperglycemia and hypoglycemia. This has the potential to change diabetes management and treatment, along with the lives of people who have to go through it.